Oxidized LDL
High Cholesterol
Nutritional Supplements Reduce Oxidized LDL Cholesterol and More! The LDL Cholesterol Level Matters Very Little Comparatively.
By Ladd McNamara, M.D.
 Discussion
Discussion
The article and protocol are for informational purposes only, and not intended as medical advice. Please read the Medical Disclaimer below, and consult with your personal physician before starting supplements and acting upon any information on this website.
Bottom Line
High LDL cholesterol is not the real problem, as it is not the main reason that people develop atherosclerosis (cardiovascular disease). The TRUE cause of cardiovascular disease is OXIDIZED LDL cholesterol, combined with arterial inflammation, that leads to arterial calcifications (plaque formation), and hardening of the arteries! It has very little to do with the actual LDL cholesterol level. Therefore, it is not necessary to be overly concerned with one’s LDL cholesterol level (as is the case in medicine), as long as the percentage of LDL cholesterol molecules that are oxidized is low, and inflammation of the arteries is kept at a minimum.
At this time, the best way to get the oxidized LDL cholesterol test, is to get it done through Life Extension. If this link does not work for you, simply type “lifeextension.com” in your browser, and then search their website for, “Oxidized LDL Blood Test.” Consider getting your OXIDIZED LDL cholesterol level checked (the test is called, “oxidized LDL”), as well as your HDL cholesterol, high-sensitivity CRP, and your homocysteine levels checked.
Cardiovascular Disease Development
 Atherosclerosis is a disease primarily initiated by oxidized LDL (low-density lipoprotein) cholesterol and inflammation of the arterial lining (endothelium). Endothelial inflammation is caused by oxidative damage from several sources, including homocysteine, a toxic amino acid intermediary, as well as cortisol (stress), high blood glucose (diabetes, metabolic syndrome), smoking, alcohol, autoimmune factors (rheumatoid arthritis, Lupus, etc.), infections, air pollution, hypoxia (e.g., sleep apnea), and excessive sun exposure. (1 – 4)
Atherosclerosis is a disease primarily initiated by oxidized LDL (low-density lipoprotein) cholesterol and inflammation of the arterial lining (endothelium). Endothelial inflammation is caused by oxidative damage from several sources, including homocysteine, a toxic amino acid intermediary, as well as cortisol (stress), high blood glucose (diabetes, metabolic syndrome), smoking, alcohol, autoimmune factors (rheumatoid arthritis, Lupus, etc.), infections, air pollution, hypoxia (e.g., sleep apnea), and excessive sun exposure. (1 – 4)
Lowering the oxidized LDL cholesterol level is key to reducing the risk for cardiovascular disease! Oxidized LDL cholesterol is not normally checked on routing lipid panels. Your doctor may not have even heard of oxidized LDL cholesterol, yet it remains one of the main factors for the development of cardiovascular disease.
If you are told you have high LDL cholesterol, and then you take a statin drug to lower it down to “acceptable” levels, how much does that lower your risk of cardiovascular disease? The reduction is minimal, and often not consistent, because there is no direct relationship between lowering your LDL cholesterol level and reducing your risk of Coronary Artery Disease (CAD).
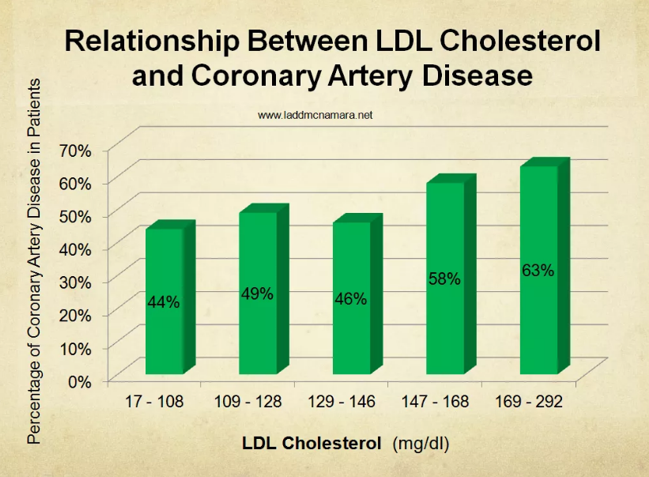
Compare that to how much your risk of cardiovascular disease can be reduced by lowering your oxidized LDL cholesterol level. There is a direct relationship of oxidized LDL cholesterol levels and CAD.

There are labs that test for oxidized LDL cholesterol, but finding them can be a chore. I used to recommend people to two different labs, but those labs were bought out by big corporate laboratory companies, and they do not offer it.
The reason that oxidized LDL cholesterol is not widely known or tested for, is that the results would suggest that YOU NEED ANTIOXIDANTS, not drugs! It would be a tacit admission that LDL cholesterol is not the real concern, but rather it is the percentage of oxidized LDL cholesterol. Ideally the oxidized LDL cholesterol percentage to that of total LDL cholesterol should be less than 10%.
Homocysteine And Plaque Formation
Homocysteine, in combination with free radicals from various sources, oxidizes the arterial lining, as well as LDL cholesterol and triglycerides, which leads to endothelial inflammation. Inflammation causes the release of C Reactive Protein (CRP), primarily from the liver— which is a known marker arterial inflammation. (5 – 7)
Homocysteine causes nicks, or cracks, in the endothelium, which is where the inflammation takes place. The LDL cholesterol molecules that are oxidized, or damaged, stick within these endothelial nicks. LDL cholesterol molecules that are not oxidized do not stick to the damaged endothelium, no matter how many LDL cholesterol molecules are present.

Oxidized LDL cholesterol molecules which are stuck within the nicks of the endothelium are then gobbled up by white blood cells, called macrophages. Macrophages gobble up more oxidized LDL cholesterol than they can handle, and eventually burst open, spilling “partially-digested” cholesterol, as if it were lard, under the arterial lining. The partially-digested cholesterol and peroxides released from the dying macrophages cause even more inflammation, which leads to calcification. In essence, this is a scarring process, which we call plaque.
The attempted healing (scarring) of the arteries continues, with plaque building up, and infiltration of smooth muscles from the arterial wall. This bulges into the lumen of the artery, causing eddy currents and reduction of blood flow. In time, arterial spasms and blood clots cause the narrowed artery to partially, or completely, close off. This may result in a stroke or heart attack, depending upon where the occluded artery is located. Usually this is happening throughout the body simultaneously.
Lowering homocysteine to less than 7 micromoles/liter (µmol/L), as well as reducing oxidized LDL cholesterol, raising HDL cholesterol, and lowering triglycerides, all with a full-range of broad spectrum, correctly-dosed pharmaceutical-grade nutritional supplement protocol, is more beneficial for reducing the risk of repeat heart attacks than any drug available. (8 – 15)
Do Not Hyper-Focus On Your LDL Cholesterol Level
 For years, doctors have hyper-focused on LDL cholesterol levels, and encouraged continually lowering them with the use of statin drugs. (Please see my article, “Heart Disease” on this website, regarding the risks and dubious benefits of statin drugs.)
For years, doctors have hyper-focused on LDL cholesterol levels, and encouraged continually lowering them with the use of statin drugs. (Please see my article, “Heart Disease” on this website, regarding the risks and dubious benefits of statin drugs.)
HDL, or high-density lipoprotein cholesterol, is responsible for clearing out the excess cholesterol in your arteries. Exercise, vitamins, minerals, essential fatty acids (fish oil), and antioxidants, particularly the bioflavonoid antioxidants, increase HDL cholesterol levels and protect the LDL cholesterol from oxidative damage, and therefore do more to reduce your risk of heart disease than any medication ever could. These factors may also lower one’s LDL cholesterol level, but that effect is secondary, even tertiary to the reduction of oxidized LDL cholesterol levels, raising HDL cholesterol, and reducing inflammation. In other words, lowering LDL cholesterol is not very important compared to the other parameter changes.
There is nothing inherently bad about LDL cholesterol. LDL cholesterol is critical to maintain life. LDL cholesterol only becomes “bad” when it is damaged, or oxidized by free radicals. Only the damaged, or oxidized form of LDL cholesterol sticks to the arterial walls to initiate the formation of plaque.(16) Studies have shown that those who had more atherosclerotic plaque were not necessarily those with higher LDL cholesterol levels, but those with higher percentages of oxidized LDL cholesterol than others. (17)
 Consider Listening to “The Cholesterol Conspiracy”
Consider Listening to “The Cholesterol Conspiracy”
To learn more about this concept, please consider listening to my audio-book, available on both iTunes and Amazon’s Audible.
To get the audio-book of “The Cholesterol Conspiracy,” from iTunes please CLICK HERE. You can also purchase it as a gift off of iTunes and email the coupon to friends and family.
Also, I think you would find Dr. Myron Wentz’s foreword to The Cholesterol Conspiracy very interesting reading. To read Dr. Wentz’s foreword to the book by CLICKING HERE.
Very Important Point Coming Up
If LDL cholesterol is not oxidized, or damaged, then it will not stick to your arterial walls to form plaque, no matter what the level. That’s good, because LDL cholesterol is GOOD, not bad. It is needed for the cells to function. In fact, you would die without it. When it goes too low, many problems arise.

Even if a person has high LDL cholesterol, they do not have to be at an increased risk of heart attack or death IF they reduce their oxidized LDL cholesterol, boost their HDL cholesterol, and reduce their homocysteine levels! This is the biggest take-away lesson!
It is critical to realize that it is not simply the level of LDL cholesterol that is the issue, it actually is the level of oxidized, or damaged LDL cholesterol that is of greatest concern. Cholesterol-lowering statin drugs do not address the true “bad” cholesterol, the oxidized LDL cholesterol.
Micronutrients Reduce Cardiovascular Disease
 The answer to lowering the life-threatening risk of arteriosclerosis, heart disease and stroke is to reduce the oxidative damage to the LDL cholesterol, triglycerides, and the arterial lining so that plaque does not form. Oxidation and disease are effectively neutralized with the use of vitamins, minerals, omega-3 fatty acids (fish oil), and other antioxidants, not with statin drugs! (18)
The answer to lowering the life-threatening risk of arteriosclerosis, heart disease and stroke is to reduce the oxidative damage to the LDL cholesterol, triglycerides, and the arterial lining so that plaque does not form. Oxidation and disease are effectively neutralized with the use of vitamins, minerals, omega-3 fatty acids (fish oil), and other antioxidants, not with statin drugs! (18)
Vitamin E is a fat-soluble vitamin. It helps protect LDL cholesterol, as well as all cell membranes in all organ tissues, from oxidative damage. Vitamin E embeds in triglycerides and cholesterol, protecting them from oxidative damage. This has been known for years, and medical studies have touted the benefits of vitamin E. Recent studies show that vitamin E, and especially the form of vitamin E, gamma tocopherol, is able to reduce the risk of heart disease and atherosclerosis beyond its antioxidant effect.
Vitamins provide protection from many diseases. (19, 20) B-complex vitamins, folic acid and B6, are associated with a reduced risk of heart attack. (21, 22) Researchers also believe that vitamin C provides protection to arterial walls and reduces plaque formation by neutralizing free radicals before they can damage elastic tissues and affect cholesterol profiles. (23 – 26) Others have studied the usefulness of a combination of antioxidants, particularly vitamins E, beta-carotene, and vitamin C in the prevention of heart disease and found them to be beneficial. (27 – 29)
 In addition, bioflavonoid antioxidants, such as quercetin, grape seed extract, and resveratrol, are associated with a reduction in many diseases, including cardiovascular disease. (30 – 37) Add to this benefits of co-enzyme Q10 and olive phenol antioxidants—and it Is obvious that the benefits are greater than any medication.
In addition, bioflavonoid antioxidants, such as quercetin, grape seed extract, and resveratrol, are associated with a reduction in many diseases, including cardiovascular disease. (30 – 37) Add to this benefits of co-enzyme Q10 and olive phenol antioxidants—and it Is obvious that the benefits are greater than any medication.
Cholesterol-lowering statin drugs reduce one’s co-enzyme Q10 levels, which in turn leads to many health problems (see my article, “Heart Disease”), is a good reason to consider not taking that class of medication. The benefits do not outweigh the risks.
The fat-soluble antioxidants, vitamin E, beta carotene, and co-enzyme Q10 ride along in the blood fat (triglycerides) and LDL cholesterol, protecting them and the endothelium from oxidation. Vitamin E embeds in the surface of LDL cholesterol, protecting it from free radical damage. Beta carotene, grape seed extract and olive extract penetrate deeper inside the LDL cholesterol and arterial walls, adding more protection from oxidation. (38) Quercetin and alpha lipoic acid work through nitrous oxide pathways to reduce high blood pressure, a major risk factor for heart disease.
Homocysteine Oxidizes LDL Cholesterol and Inflames Arteries
The B vitamins, particularly vitamin B12, along with betaine, a.k.a., tri-methyl-glycine (TMG), change homocysteine into a safer amino acid, methionine, by adding a methyl group, and reduce inflammation of the LDL cholesterol and the arterial lining. Studies published in the Journal of the American Medical Association (JAMA) and the New England Journal of Medicine (NEJM) have shown that lowering homocysteine levels with the B vitamins significantly reduces the risk of heart disease and heart attacks. (39 – 43)
Studies have shown how the B-complex vitamins, particularly folic acid, vitamin B6, and vitamin B12 help reduce homocysteine levels by facilitating the conversion of homocysteine into cysteine.(44, 45) This leaves less homocysteine to oxidize and nick the arterial walls and LDL cholesterol. To further reduce homocysteine levels, one can take the amino acid betaine, also known as tri-methyl-glycine (TMG), as it “back-converts” homocysteine into methionine.

When you receive the results of your homocysteine test, do not accept the answer, “Your test was normal.” Ask for the actual number. The doctor and nurse usually know what is normal by what the lab report states as the “normal range.” Most lab results report a normal homocysteine level as being below 10.4 µmol/L, when in fact, since the early 1990’s, researchers have known that a homocysteine count above 6.5 µmol/L signals a rapid linear rise in the risk for heart disease.
Furthermore, for every 3-point elevation of homocysteine above 6.5 µmol/L, e.g., when homocysteine levels are 9.5 µmol/L, the risk of coronary artery disease (CAD) rises by an additional 35%! Yet you may be told that 9.5 µmol/L is “normal and not to worry.” With a homocysteine level of 12.5 µmol/L, the increase in the risk for heart disease exceeds 70%.
The greater the homocysteine level, the greater the oxidation of both LDL cholesterol and the arterial lining. The greater the inflammation, the higher the CRP. Is it any wonder that homocysteine and CRP levels are more predictive for risk of heart disease than cholesterol levels and ratios? (46, 47)
Those who have looked at the studies will have seen that by lowering the percentage of oxidized cholesterol, no matter the actual level of LDL cholesterol, along with raising HDL cholesterol, and lowering homocysteine below 6.5 µmol/L, all with nutritional supplements, a person reduces their risk of heart disease and stroke far greater than by using any drug.
Grape Seed Extract and Vitamin C
 Vitamin C intake is associated with a decreased risk of heart disease. (48, 49) One study found that the risk of death from cardiovascular disease was 42% lower in men and 25% lower in women who consumed more than 300 mg/day of vitamin C. (50) Recent results from the Nurses’ Health Study, based on the follow-up of more than 85,000 women over a sixteen-year period, also suggest that higher vitamin C intakes may be cardio-protective. (51)
Vitamin C intake is associated with a decreased risk of heart disease. (48, 49) One study found that the risk of death from cardiovascular disease was 42% lower in men and 25% lower in women who consumed more than 300 mg/day of vitamin C. (50) Recent results from the Nurses’ Health Study, based on the follow-up of more than 85,000 women over a sixteen-year period, also suggest that higher vitamin C intakes may be cardio-protective. (51)
Vitamin C and grape seed extract in combination are very powerful in preventing oxidation in all areas — the LDL cholesterol, the endothelium, and deeper in the arterial walls. Furthermore, vitamin C replenishes grape seed extract and vitamin E, and thereby synergistically protects LDL cholesterol and the arterial walls better than any of them separately.
Vitamin K2 Helps With The Proper Placement of Calcium
Vitamin K2 helps mobilize calcium out of the arterial walls and drives it back into the bones where it belongs. When a person has osteoporosis and arterial calcifications, I prescribed higher doses of vitamin K2, e.g., 360 – 2000 mcg per day. Blood calcium levels will remain constant, but the decrease in arterial wall calcifications will reduce the hardening of the arteries, and the bones will be strengthened.
In fact, when a person is supplementing with high doses of vitamin D3 (> 1000 IU/day), it is important to also supplement with vitamin K2. One should consider taking 45 mcg per day for every 1000 IU of vitamin D3 that is being consumed. For example, if one is taking 2000 IU per day, as in a quality nutritional vitamin-antioxidant tablet, consider taking at least 90 mcg/day (or more) of vitamin K2 (in the MK-7 form). If one is taking 10,000 IU per day of vitamin D3, then consider taking at least 450 mcg of vitamin K2 per day.
Flavonoid Antioxidants Help Reduce LDL Oxidation and Cardiovascular Disease
The bioflavonoid class of antioxidants, that include among many others, grape seed extract, resveratrol, and quercetin just to name a few, is associated with reducing the risk of heart attack and stroke by as much as 50% and possibly as high as 70%. (52, 53) Grape seed extract is one of the more potent antioxidants that neutralize free radical oxidation of LDL cholesterol, the arterial lining, the arterial wall, the liver, the brain, the kidneys, and the skin. Both grape seed extract and quercetin work synergistically with other antioxidants, and even more so with resveratrol, also from red grapes.
Resveratrol can lower LDL cholesterol levels, but it is the reduction of oxidized LDL cholesterol that has the greater effect on preventing atherosclerosis.(54) Supplementation with a combination of grape seed extract and resveratrol work synergistically to reduce LDL cholesterol levels, Apo-protein B levels, oxidized LDL cholesterol levels, and raise HDL cholesterol levels. (55) The combination of these two antioxidants derived from the red grape work better together to have this dual effect than either micronutrient can do alone.
Green Tea Extract and Olive Extract
Green tea extract helps to both reduce the oxidation of LDL cholesterol and to lower LDL cholesterol.(56) This is more helpful than just lowering LDL cholesterol as with prescription drugs. Green tea extract also reduces the oxidation of the arterial endothelium. Green tea extract not only increases HDL cholesterol, it helps prevent cancer.
 Olive oil and olive extract bestow incredible health benefits. There are powerful phenol antioxidants within the fruit of olives that are associated with a significant decreased risk of heart attack and cancer. The Mediterranean diet, in which olive oil is the primary source of fat, has been shown to provide the longest lifespan and lowest incidence of heart disease and cancers compared to other diets. (57 – 59)
Olive oil and olive extract bestow incredible health benefits. There are powerful phenol antioxidants within the fruit of olives that are associated with a significant decreased risk of heart attack and cancer. The Mediterranean diet, in which olive oil is the primary source of fat, has been shown to provide the longest lifespan and lowest incidence of heart disease and cancers compared to other diets. (57 – 59)
Many studies have shown olive oil reduces death from heart disease by reducing atherosclerosis, plaque formation, lowering LDL cholesterol, preventing oxidation of LDL cholesterol, raising HDL cholesterol, and preventing abnormal and potentially lethal clot formation. (60 – 68)
Alpha-lipoic acid protects against oxidative damage to LDL cholesterol and reduces the inflammatory cellular response within arterial walls that produces more oxidative damage and plaque formation. (69) Alpha-lipoic acid, along with magnesium, is able to prevent and help reduce high blood pressure in diabetics. This is accomplished by raising the levels of glutathione to protect bio-mechanisms that regulate arterial tone. (70, 71)
The combination of alpha-lipoic acid (ALA), vitamin E, grape seed extract, olive extract, green tea extract, quercetin, resveratrol, turmeric extract, and Co-Q10 synergistically work together in the prevention of oxidation of LDL cholesterol and the arteries much better than any of these working alone. (72)
Fish Oil (Omega-3 Fatty Acids)
 Omega-3 essential fatty acids as from fish oil, especially a quality brand that is ensured to provide concentrated levels of both DHA (docosahexaenoic acid) and EPA (eicosapentaenoic acid), helps reduce oxidation of LDL cholesterol and arterial inflammation, which means a reduction cardiovascular disease.(73)
Omega-3 essential fatty acids as from fish oil, especially a quality brand that is ensured to provide concentrated levels of both DHA (docosahexaenoic acid) and EPA (eicosapentaenoic acid), helps reduce oxidation of LDL cholesterol and arterial inflammation, which means a reduction cardiovascular disease.(73)
Most commercially-available fish oil supplements consist primarily of EPA, and less DHA. Yet scientific evidence shows it is the DHA component that is more effective in preventing heart disease. (74, 75) Worse, is the concern of mercury – which is more of a problem with eating fish. The best advice I can give is to use a pure fish oil brand with concentrated DHA levels, manufactured to standards that eliminate contaminants, such as BCP’s and dioxins.
In a study consisting of 11,323 people who had suffered a heart attack within the previous three months, fish oil supplements (850 mg of EPA & DHA) were shown to reduce the risk of sudden death and repeat heart attacks by 45%, and provide a 20% decrease in total mortality, versus placebo. (75)
Fish oil is an omega-3 fatty acid that gets incorporated into cholesterol and triglycerides and prevents the oxidation of LDL cholesterol. Since LDL cholesterol is protected from excessive oxidation there is less plaque buildup, and less risk of heart disease. (76 )
C Reactive Protein
 The Framingham Cohort study, among many others, revealed that high levels of CRP are associated with the severity of coronary artery calcifications, i.e., atherosclerosis.(77, 78) Even in the presence of no other risk factors, people with the highest levels of CRP have five times the risk of developing atherosclerosis, and five times the risk of having a heart attack compared to those with lower levels. (79, 80)
The Framingham Cohort study, among many others, revealed that high levels of CRP are associated with the severity of coronary artery calcifications, i.e., atherosclerosis.(77, 78) Even in the presence of no other risk factors, people with the highest levels of CRP have five times the risk of developing atherosclerosis, and five times the risk of having a heart attack compared to those with lower levels. (79, 80)
Antioxidants, including vitamin E, vitamin C, grape seed extract, resveratrol, turmeric extract, green tea extract, olive extract, fish oil, and more reduce inflammation and CRP levels, and therefore, a marker for the risk of cardiovascular disease is lowered. The best way to get rid of oxidation, or inflammation, is with antioxidants. If statin drugs were to work at all, it would be because they lower inflammation (a little), not due to their ability to lower LDL cholesterol. (81, 82)
Lab Tests
Consider getting at least these tests:
• Oxidized LDL (You will have to find a lab to get this test.)
• HDL Cholesterol
• Triglycerides
• Homocysteine
• C Reactive Protein (High Sensitivity)
At this time, the best way to get the oxidized LDL cholesterol test, is to get it done through Life Extension. If this link does not work for you, simply type “lifeextension.com” in your browser, and then search their website for, “Oxidized LDL Blood Test.” Consider getting your OXIDIZED LDL cholesterol level checked (the test is called, “oxidized LDL”), as well as your HDL cholesterol, high-sensitivity CRP, and your homocysteine levels checked.
To Learn More About This Concept, Please Consider Listening to My Audio-Book, available on both iTunes and Audible.
 To get the audio book of “The Cholesterol Conspiracy,” from iTunes please CLICK HERE. If this link to iTunes does not work for you, simply click here, laddmcnamara.com, to go to my main website, and then click on the image of The Cholesterol Conspiracy book within that article, and that will redirect to iTunes. It is that article where you can read the foreword by Dr. Myron Wentz’s: CLICK HERE.
To get the audio book of “The Cholesterol Conspiracy,” from iTunes please CLICK HERE. If this link to iTunes does not work for you, simply click here, laddmcnamara.com, to go to my main website, and then click on the image of The Cholesterol Conspiracy book within that article, and that will redirect to iTunes. It is that article where you can read the foreword by Dr. Myron Wentz’s: CLICK HERE.
Please read Dr. Myron Wentz’s foreword to this book by CLICKING HERE.
Supplement Protocol for Cardiovascular Disease and/or High Cholesterol
The article and protocol are for informational purposes only, and not intended as medical advice. Please read the Medical Disclaimer below, and consult with your personal physician before starting supplements and acting upon any information on this website.
Minimal Protocol to Protect LDL Cholesterol and Arteries

Basic Protocol to Protect LDL Cholesterol and Arteries

Average Protocol to Protect LDL Cholesterol and Arteries

Advanced Protocol to Protect LDL Cholesterol and Arteries

- AM: With, or after breakfast
- Noon: At lunchtime with food, or shortly thereafter
- PM: Late afternoon with food, or at, or after dinner
- Please see my list of ingredients (below) that I like to see provided by a foundational vitamin and mineral supplement.
- Booster Antioxidant Supplement, with each tablet providing 50 mg Pterocarpus marsupium extract (containing pterostilbene), 10 mg Olive Fruit Extract, 75 mg alpha lipoic acid (ALA), and 60 mg Quercetin.
- A quality liver support supplement, that provides milk thistle extract, N-acetyl-L-cysteine, alpha lipoic acid, broccoli extract, curcumin (turmeric extract), olive extract, green tea extract, and biotin, not only supports all liver functions, it also helps reduce LDL cholesterol, prevent LDL cholesterol from oxidative damage, support heart health, as well as supports brain and eye health, and helps fight cancer cells.
- Beta glucan polysaccharides, derived from the membranes of the shiitake and reishi mushrooms, as well as baker’s yeast extract, not only support cardiovascular health, they also support improved blood glucose, mood, and supports the immune system to kill viruses, bacteria, yeast, and cancer cells. It also is powerful in protecting against infection by viruses, by inhibiting viruses from connecting with host cells. They also help maintain healthy cholesterol.
- A quality vision support supplement not only supports eye health (by preventing cataract formation, macular degeneration, and improving visual acuity and night vision), it also helps support improved cardiovascular health, and brain health.
- Probiotics, at least take 12 billion colony-forming bacteria, providing Lactobacillus rhamnosus LGG® and Bifidobacterium BB12®, every other day or daily.
- As for the Homocystrol + TMG, Methylated Resveratrol Plus, D-Ribose, Acetyl-L-Carnitine, and DHEA, these are not carried by the preferred supplement manufacturer. You you can buy these from Douglas Labs, by first creating a customer account by CLICKING HERE. (If this link does not work for you, simply type “douglaslabs.com/patient-account” into a new browser tab.) And, please use Referral Code 2074214.
- Homocystrol + TMG (SKU# 201329-90X)
- Methylated Resveratrol Plus (SKU# 200901-30X)
- Corvalen (or D-Ribose; SKU# 57452P-340X)
- Acetyl-L-Carnitine (SKU# 82730)
- DHEA, 25 mg, micronized (SKU# 83050)
Ingredients that I like to see provided collectively by vitamin-antioxidant & chelated mineral tablets
Vitamin A, mostly as Beta Carotene
Vitamin C
Vitamin D3
Vitamin E
Vitamin K (K1 & K2)
B-Complex Vitamins
Curcumin (turmeric extract)
Quercetin
Green Tea Extract
Olive Extract
Rutin
Resveratrol
Choline
Lutein
Lycopene
N-Acetyl-L-Cysteine (NAC)
Calcium
Magnesium
Iodine (as potassium iodide)
Zinc
Selenium
Copper
Manganese
Chromium
Molybdenum
Including Ultra Trace Minerals
Medical Disclaimer:
Information on this website, written, spoken, or in any other communication by Dr. Ladd McNamara or any other information or reference is for informational purposes only. The information provided on this website is a result of years of practice, experience, and study by the author. This information is not intended as a substitute for the advice provided by someone’s personal licensed physician or other healthcare professional, or any information contained on or in any product label or packaging. Do not use the information on this website, or any other form of communication from Dr. Ladd McNamara or the Dr. Ladd VIP Program, for diagnosing or treatment of a health issue or disease, or for the prescribing of medication or the use of supplementation without a discussion with your licensed health professional first. At best, the information provided on this website is only meant to supplement information provided by your own doctor or health professional, not to replace medical advice. The information from this website is not meant to cover all possible uses, precautions, interactions or possible adverse effects of nutritional supplements with or without medications, or in conjunction with specific medical conditions. The information from this website may not fit your specific health circumstances. Never delay seeking medical care or disregard advice from your health care professional because of information you have received directly or indirectly from this website, from the Dr. Ladd VIP Program, or from Dr. Ladd McNamara himself. Always speak with your physician or other healthcare professional before making any changes to your medication or embarking on a nutritional, herbal or homeopathic supplement program, or before using any treatment for a health concern. If you have, or suspect that you have, a medical problem, contact your health care provider promptly. Do not disregard professional medical advice or delay in seeking professional advice because of something you have read or heard on this website, or due to any other information from Dr. Ladd McNamara or his representatives. Information provided on this website or the V.I.P. Program, and the use of any products or services mentioned on this website (or as a result of information provided this program, article, or website) by you DOES NOT create a doctor-patient relationship between you and Ladd McNamara, M.D. Information and statements regarding dietary supplements have not been evaluated by the Food and Drug Administration and are not intended to diagnose, treat, cure, or prevent any disease.
References
- Schroecksnadel K, et al. Crucial role of interferon-gamma and stimulated macrophages in cardio-vascular disease. Curr Vasc Pharmacol. 2006 Jul;4(3):205-13.
- Gibelin P, et al. Prognostic value of homocysteinemia in patients with congestive heart failure. Clin Chem Lab Med. 2006;44(7):813-6.
- Van Oijen MG, et al. Hyperhomocysteinaemia and Vitamin B12 Deficiency: The Long-Term Effects in Cardiovascular Disease. Cardiology. 2006 Jun 6;107(1):57-62 [Epub ahead of print].
- Castellon X., Bogdanova, V. Chronic Inflammatory Diseases and Endothelial Dysfunction. Aging Dis. 2016 Jan; 7(1): 81–89.
- Haim M, et al. Serum Homocysteine and Long-Term Risk of Myocardial Infarction and Sudden Death in Patients with Coronary Heart Disease. Cardiology. 2006 Jun 6;107(1):52-56.
- Laaksonen R, et al. High oxidized LDL and elevated plasma homocysteine contribute to the early reduction of myocardial flow reserve in healthy adults. Eur J Clin Invest. 2002 Nov;32(11):795-802.
- Troughton JA, et al. Homocysteine and coronary heart disease risk in the PRIME study. Atherosclerosis. 2006 Jun 13; [Epub ahead of print].
- Fuller C, Jialal I, et al. rrr-alpha-tocopherol acetate supplementation at pharmacologic doses decreases low-density-lipoprotein oxidative susceptibility but not protein glycation in patients with diabetes mellitus. Am J Clin Nutri. 1996 63:753-759.
- Somogyi A, et al. Hypothetical connection between diabetes mellitus and free radical reactions in arteriosclerosis. Orvosi Hetilap [Hungarian] 1994 135:(33):1815-1818.
- Jialal I. Effect of combined supplementation with alpha-tocopherol ascorbate and beta-carotene on low-density lipoprotein oxidation. Circulation. 1993 88:2780-2786.
- Street D, et al. A population based case control study of the association of serum antioxidants and myocardial infarction. Am J Epidemiol. 1991 134:719-720.
- Steinberg D, et al. Antioxidants in the prevention of human atherosclerosis. Circulation. 1992 85:6:2338-2343.
- Gey K, et al. Inverse correlation between plasma vitamin E and mortality from ischemic heart disease in cross-cultural epidemiology. Am J Clin Nutri. 1991 53:326S-334S.
- Stampfer M, et al. Vitamin E consumption and the risk of coronary disease in women. New Engl J Med. 1993 328:1444-1449.
- Rimm E, Stampfer M, et al. Vitamin E consumption and the risk of coronary artery disease in men. New Engl J Med. 1993 328:1450-1456.
- Tsimikas, S, et al. Oxidized phospholipids, Lp(a) lipoprotein, and coronary artery disease. N Engl J Med. 2005 Jul 7;353(1):9-11.
- Anselmi M, et al. Plasma levels of oxidized-low-density lipoproteins are higher in patients with unstable angina and correlated with angiographic coronary complex plaques. Atherosclerosis. 2006 Mar;185(1):114-20.
- Aviram M. HDL–associated paraoxonase 1 (PON1) and dietaryantioxidants attenuate lipoprotein oxidation, macrophage foam cells formation and atherosclerosis development. Pathophysiol Haemost Thromb. 2006;35(1-2):146-51.
- Mehra M, et al. Prevention of atherosclerosis. Postgraduate Med. 1995 98:1:175-182.
- Hoffman RM, et al. Antioxidants and the prevention of coronary heart disease. Arch Int Med. 1995 155:241-244.
- Morrison H, et al. Serum folate and risk of fatal coronary heart disease. J Am Med Assoc. 1996 275:24:1893-1896.
- Chasan-Taber L, et al. A prospective study of folate and vitamin B-6 and risk of myocardial infarction in U.S. physicians. J Am Coll Nutri. 1996 15:2:136-143.
- Levine GN, et al. Ascorbic acid reverses endothelial vasomotor dysfunction in patients with coronary artery disease. Circulation. 1996 93:6:1107-1113.
- Gatto LM, et al. Ascorbic acid induces a favorable lipoprotein profile in women. J Am Coll Nutri. 1996 15:2:154-158.
- Hallfrisch J, et al. High plasma vitamin c associated with high plasma HDL (1) – and HDL (2) cholesterol. Am J Clin Nutri. 1994 60:100-105.
- Osganian S, Stampfer M, Rimm E, Spiegelman D, et al. Vitamin C and risk of coronary heart disease in women. J Am Coll Cardiol. 2003 42:246-252.
- Rifici V, Khachadurian A. Dietary supplementation with vitamins C and E inhibits in-vitro oxidation of lipoproteins. J Am Coll Nutri. 1993 12:6:6331-6337.
- Gaziano J. Antioxidant vitamins and coronary artery disease risk. Am J Med. 1994 97:3A-18S-3A-21S.
- Lagrue G, et al. A study of the effects of procyanidol oligomers on capillary resistance in hypertension and in certain nephropathies. Sem Hop Paris. 1981 57:1399-1401.
- Detre A, et al. Studies on vascular permeability in hypertension: action of anthocyanosides. Clin Physiol Biochem. 1986 4:143-149.
- Meunier MT, et al. Free-radical scavenger activity of procyanidolic oligomers and anthocyanosides with respect to superoxide anion and lipid peroxidation. Plant Medphytother. 1989 4:267-274.
- Tixier J, et al. Evidence by in vivo and in vitro studies that binding of pycnogenols to elastin affects its rate of degradation by elastases. Biochem Parmacol. 1984 33:3933-3939.
- Facino R, et al. Free-radical scavenging action and anti-enzyme activities of procyanidines from vitis vinifera; a mechanism for their capillary protective action. Arzneimittel-Forschung Drug Research. 1994 44(1):5:592-601.
- Dartenuc JY, et al. Capillary resistance in the geriatric: study of a micro-angioprotector. Bordeaux Medicale. 1985 13:903.
- Kuhnau J. The flavonoids, a class of semi-essential food components: their role in human nutrition. World Rev Nutr Diet. 1976 24:117-191.
- Gabor M. Pharmacologic effects of flavonoids on blood vessels. Angiologica, 1972 9:355-374.
- Knekt P, et al. Flavonoid intake and coronary mortality in finland: a cohort study. Brit Med J. 1996 312:478-481.
- Niki E, et al. Interaction among vitamin C, vitamin E, and beta carotene. Am J Clin Nutri. 1995 62(suppl):1322S-1326S.
- Nestel P, et al. The n-3 fatty acids eiosapentaenoid acid and docosahexaenoic acid increase systemic arterial compliance in humans. Am J Clin Nutr 2002 Aug;76(2):326-330.
- Morrison H, et al. Serum folate and risk of fatal coronary heart disease. JAMA 1996 Jun 26;275:1893-1896.
- Graham I, Daly L, Refsum H, et al. Plasma homocysteine as a risk factor for vascular disease. The European Concerted Action Project. JAMA. 1997 277:1775-1781.
- McCully K. Homocysteine, folate, vitamin B6, and cardiovascular disease (Editorial). JAMA. 1998 279:392-393.
- Wald N, Watt H, Law M, Weir D, McPartlin J, Scott J. Homocysteine and ischemic heart disease: results of a prospective study with implications regarding prevention. Arch Intern Med. 1998 158:862¬-867.
- Chasan-Taber L, et al. A prospective study of folate and vitamin B-6 and risk of myocardial infarction in U.S. physicians. J Am Coll Nutri. 1996 15:2:136-143.
- Morrison H, et al. Serum folate and risk of fatal coronary heart disease. J Am Med Assoc. 1996 275:24:1893-1896.
- Nygard O, Nordrehaug J, Refsum H, et al. Plasma homocysteine levels and mortality in patients with coronary artery disease. NEJM 1997 337:230-236.
- Luc G, Bard J, Juhan-Vague I, et al. C-reactive protein, interleukin-6, fibrinogen as predictors of coronary heart disease. The PRIME study. Arterioscler Thromb Vasc Biol. 2003 Jul 1;23(7):1255-1261.
- Carr A, Frei B. Toward a new recommended dietary allowance for vitamin C based on antioxidant and health effects in humans. Am J Clin Nutr. 1999 69(6):1086-1107.
- Osganian S, Stampfer M, Rimm E, Spiegelman D, et al. Vitamin C and risk of coronary heart disease in women. J Am Coll Cardiol. 2003 42:246-252.
- Enstrom J. Counterpoint–vitamin C and mortality. Nutr Today. 1993 28:28-32.
- Osganian S, Stampfer M, Rimm E, et al. Vitamin C and risk of coronary heart disease in women. J Am Coll Cardiol. 2003 42(2):246-252.
- Hertog M, Feskens E, Hollman P, Katan M, Kromhout D. Dietary antioxidant flavonoids and risk of coronary heart disease: the Zutphen Elderly study. Lancet 1993 Oct 23;342(8878):1007-1011.
- Keli S, et al. Dietary flavonoids, antioxidant vitamins, and incidence of stroke: the Zutphen study. Arch Intern Med 1996 Mar 25;156(6):637¬642.
- Haim M, et al. Serum Homocysteine and Long-Term Risk of Myocardial Infarction and Sudden Death in Patients with Coronary Heart Disease. Cardiology. 2006 Jun 6;107(1):52-56.
- Bonaa KH, et al. Homocysteine lowering and cardiovascular events after acute myocardial infarction. N Engl J Med. 2006. Apr 13;354(15):1578-88.
- Maron D, Lu G, Cai N, et al. Cholesterol-lowering effect of a theaflavin-enriched green tea extract. A randomized controlled trial. Arch Intern Med. 2003;163:1448-1453.
- Owen RW, et al. Olive oil consumption and health: the possible role of antioxidants. Lancet Oncol, 2000, Oct., 1:107-12.
- Visioli F, et al. Antioxidant and other biological activities of phenols from olives and olive oil. Med Res Rev. 2002 Jan;22(1):65-75.
- Simopoulos Ap. The traditional diet of Greece and cancer. Eur J Cancer Prev. 2004 Jun;13(3):219-30.
- Visioli F., et al. Low density lipoprotein oxidation is inhibited in vitro by olive oil constituents. Atherosclerosis. 1995 Sep;117(1):25-32.
- Cullinen K. Olive oil in the treatment of hypercholesterolemia. Med Health R.I. 2006 Mar;89(3):113.
- Nagyova A, et al. Effects of dietary extra virgin olive oil on serum lipid resistance to oxidation and fatty acid composition in elderly lipidemic patients. Bratisl Lek Listy. 2003;104(7-8):218
- Martinez-Gonzalez MA. The SUN cohort study (Seguimiento University of Navarra). Public Health Nutr. 2006 Feb;9(1A):127-31.
- Bogani P., et al. Postprandial anti-inflammatory and antioxidant effects of extra virgin olive oil. Atherosclerosis. 2006 Feb 17; [Epub ahead of print].
- Fito M., et al. Antioxidant effect of virgin olive oil in patients with stable coronary heart disease: a randomized, crossover, controlled, clinical trial. Atherosclerosis. 2005 Jul;181(1):149-58.
- Fernandez-Jarne E., et al. Risk of first non-fatal myocardial infarction negatively associated with olive oil consumption: a case-control study in Spain. Int J Epidemiol. 2002, Apr;31(2):474-80.
- Visioli F., Galli C. Antiatherogenic components of olive oil. Curr Atheroscler Rep. 2001. Jan;3(1):64-7.
- Visioli F., et al. Low density lipoprotein oxidation is inhibited in vitro by olive oil constituents. Atherosclerosis. 1995 Sep;117(1):25-32.
- Zhang WJ, Frei B. Alpha-lipoic acid inhibits TNF-alpha-induced NF-kappa B activation and adhesion molecule expression in human aortic endothelial cells. FASEB J 2001 Nov;15(13):2423-2432.
- El Midaoui A, de Champlain J. Prevention of hypertension, insulin resistance, and oxidative stress by alpha-lipoic acid. Hypertension 2002 Feb;39(2):303-307.
- Takaoka M, et al. Effects of alpha-lipoic acid on deoxycorticos-terone acetate-salt-induced hypertension in rats. Eur J Pharmacol 2001 Jul;20;424(2):121-129.
- Gonzalez-Perez O, Gonzalez-Castaneda R, Huerta M, et al. Beneficial effects of -lipoic acid plus vitamin E on neurological deficit, reactive gliosis and neuronal remodeling in the penumbra of the ischemic rat brain. Neuroscience Letters, 2002 March 15, 321(5);1:100-104.
- Nestel P, et al. The n-3 fatty acids eiosapentaenoid acid and docosahexaenoic acid increase systemic arterial compliance in humans. Am J Clin Nutr 2002 Aug;76(2):326-330.
- McLennan O. Myocardial membrane fatty acids and the antiarrhythmic actions of dietary fish oil in animal models. Lipids 2001 36 Suppl: S111-S114.
- Marchioli R, Barzi F, Bomba E, et al. Early protection against sudden death by n-3 polyunsaturated fatty acids after myocardial infarction: time-course analysis of the results of the Gruppo Italian per lo Studio dells Soprvvivenza nell’Infarto Micardico (GISSI)-Prevenzione. Circulation. 2002 Apr 23;105:1897-1903.
- Bernier M, et al. Reperfusion-induced arrhythmias and oxygen-derived free radicals. Circulation Res. 1986 58:331-340.
- Guetta J, Fuselli J, Boissonnet C, Fairman E, et al. Pognostic value of C-reactive protein in diabetic patients with unstable angina. Am Coll Cardiol. 2003 41:346.
- Wang TJ, et al. C-reactive protein is associated with subclinical epicardial coronary calcification in men and women: the Framingham Heart Study. Circulation 2002 Sep 3;106(10):1189-1191.
- Ziaris M, et al. C-reactive protein and multiple complex coronary artery plaques in patients with primary untstable angina. Atherosclerosis 2002 Oct;164(2):355.
- Pradhan AD, et al. Inflammatory biomakers, hormone replacement therapy, and incident coronary heart disease: propective analysis from the Women’s Health Initiative observational study. JAMA 2002 Aug 28;288(8):980-987.
- Ridker PM, et al. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. NEJM 1997 Apr 3;336(14):973-979.
- Kaplan RC, Frishman WH. Systemic inflammation as a cardiovascular disease risk factor and as a potential target for drug therapy. Heart Dis 2001 Sep-Oct;3(5):326-332.
- Zhang Y, Zhang Y. Pterostilbene, a novel natural plant conduct, inhibits high fat-induced atherosclerosis inflammation via NF-κB signaling pathway in Toll-like receptor 5 (TLR5) deficient mice. Biomed Pharmacother. 2016 Jul;81:345-355.
- Tang T, et al. Pterostilbene reduces endothelial cell injury in vascular arterial walls by regulating the Nrf2-mediated AMPK/STAT3 pathway in an atherosclerosis rat model. Exp Ther Med. 2020 Jan; 19(1): 45–52.
- Zhang L, et al. Pterostilbene protects vascular endothelial cells against oxidized low-density lipoprotein-induced apoptosis in vitro and in vivo. Apoptosis. 2012 Jan;17(1):25-36.
All materials on this website, written, audio, visual, are copyrighted by Ladd McNamara, Inc., and are not to be distributed, duplicated, shared, posted to another website or social media sites (including Facebook, etc.), except for under the Terms of Use for sharing approved articles and videos.
As a VIP member, you agree that you will NOT share any written, audio, video, or any other proprietary materials from this website with those in your organization, other associates, or team members; and that you will only share approved articles/protocols and videos with your OWN PERSONAL & IMMEDIATE customers, clients, and prospective customers/clients. Doing so, would result in the loss of your Dr. Ladd VIP membership without a refund.
Thank you for your honesty and integrity.
About the Dr. Ladd VIP Program
There are many more articles on various subjects, as well as videos on health concerns, along with specific nutritional supplement protocols for managing health concerns and disease. Of course, this is all for informational purposes, and not to be taken as medical advice. (See medical disclaimer above.) Please learn more at www.drladdvip.com.
Please read about the benefits of being a Dr. Ladd VIP Member. It is a subscription-based personal program to better your health, energy, and passion for life, and for helping others. This program includes on-going support for yourself, and as you help customers and clients with your health enterprise.
Do you have a need to understand how NUTRITIONAL SUPPLEMENTS can benefit the health of people suffering from any number of chronic diseases; such as Heart Disease, Cancer, Diabetes, Arthritis, Dementia, Lyme Disease, Autoimmune Diseases, and Many More!
- Do you have a need for SUPPLEMENT PROTOCOLS as to what specific supplement combinations to use?
- How about WHY SUPPLEMENTS? How do you chose a QUALITY BRAND?
- Do you have a need to BETTER ASSIST CUSTOMERS in making a good decision?
- How about ON-GOING SUPPORT for ON-GOING QUESTIONS?
- How about YOUR PERSONAL HEALTH, and/or Your PERSONAL RELATIONSHIPS?
Happiness and Health includes not only being free of disease, but passionately engaged in a relationship, in life, and in helping others! It means living with less stress, more fun, and activity.
The Dr. Ladd VIP Program is about Vitality, Intimacy, and Passion, being balanced in all aspects of life, and helping others to get there too.

Please read more at www.drladdvip.com, and take advantage of the Video Courses, the Supplement Protocols, Articles, Downloadable PDFs, and Dr. Ladd VIP Facebook Community and Support. “Have me in your back pocket” by becoming a VIP Member Today!
If you are not a VIP member, please subscribe to my email list. If you are already a VIP member, no need to subscribe to the email newsletter list. Thank you.
dr. ladd
Please learn more about the Dr. Ladd VIP program here: www.drladdvip.com.
Please Subscribe to Dr. Ladd’s Email List
Receive health and website updates, as well as information on upcoming FREE health-related webinars.
All information, written or video, is copyrighted by Ladd McNamara, Inc., and is not to be shared, duplicated, or posted to other websites or social media platforms without express permission from Ladd McNamara, M.D. Thank you.
Dr. Ladd’s V.I.P. Program and Website is Owned and Operated by Ladd R. McNamara, M.D. and Ladd McNamara, Inc., a California corporation. 2020
